Orchiectomy
And how to do it yourself
What is it?
Orchiectomy, orchie for short, is a surgical procedure in which one or both testicles are removed1. For our purposes there are two viable types of orchiectomy – inguinal2, where the incision through which testicles are removed is made on the abdomen, and simple orchiectomy where the incision is made on the scrotum. Simple orchiectomy can either be done with a single midline incision along the raphe or with bilateral incisions on either side and perpendicular to the raphe.
Inguinal orchiectomy is a more invasive, risky and complicated procedure although it is possible that the end result is better aesthetically. Nowadays it is rarely performed on transgender patients. Another important aspect to consider is the possibility that a patient may want SRS (bottom surgery) in the future, where in some procedures the scrotum is used for the creation of the neovagina. A simple orchiectomy using a bilateral incision is likely to scar the scrotum and will cause some surgeons to refuse to perform an SRS procedure; conversely, the raphe is often cut and discarded. For these reasons simple orchiectomy using midline incision is believed to be the preferred method3 and is what the rest of the document shall focus on.
Anatomy
It is first important to understand the basic anatomy of the scrotum456.
Externally, the scrotum looks like a single pouch of skin separated into lateral portions by a median ridge called the raphe. Internally, the scrotal septum divides the scrotum into two compartments, each containing a single testis. The septum is made up of a subcutaneous layer and muscle tissue called the dartos muscle, which is composed of bundles of smooth muscle fibres. The dartos muscle is also found in the subcutaneous layer of the scrotum. Associated with each testis in the scrotum is the cremaster muscle (suspender), a series of small bands of skeletal muscle that descend as an extension of the internal oblique muscle through the spermatic cord to surround the testes.
There are also several membrane layers (called fascia) of the scrotal wall, with the tunica vaginalis surrounding the testis itself. The tunica vaginalis is comprised of the visceral and parietal layers, with the cavity between them being the tunica vaginalis cavity. There is some fluid in the cavity between the two layers helping with the movement of the testis in the scrotum.
The spermatic cord primarily consists of a thick hard tube called the vas/ductus deferens (the sperm duct), the testicular artery and a network of testicular veins called the pampiniform plexus. In surgical practice, the vas deferens and the vascular bundle can be separated.
Dissection videos:
“12: Dissection of Scrotum”
www.youtube.com/watch?v=jyuFbJRsNDM
“13: Dissection of coverings of spermatic cord and testis”
www.youtube.com/watch?v=bCeqzKltGJI
“14: Dissection of spermatic cord”
www.youtube.com/watch?v=JJjjyumIJOY
“Anatomy Dissection of Testis”
www.youtube.com/watch?v=DQOrBd8vn0w
Procedure
A number of resources were consulted for the writeup of the procedure78910. Additionally, a range of orchiectomy videos are available on YouTube (see end of document).
The surgical room should be warm to avoid heat loss of the patient and reduce risk of infection. Surgery should be undertaken during daytime to prevent fatigue and the surgeon should be well-rested. A battery-powered light source (or daylight) should be present to avoid any potential issues cause by power outage. In the case of self-surgery, there must be an additional person present in the case of emergency and emergency services should be available at short notice. Do not take aspirin or other blood thinning medication for at least a week prior to surgery..
Asepsis
Prior to surgery, all surgical instruments should be sterilised1112. The most effective method for this is steam under high temperature and pressure for ~40 minutes which can be achieved via the use of an autoclave (or a commercial pressure cooker1314), followed by dry hot air for ~2 hours (via the use of a sterile oven). Alternative methods include an isopropyl alcohol bath, dilute bleach solution, hydrogen peroxide or similar oxidative/bactericidal treatments. Some instruments such as needles, syringes, scalpel blades and suturing materials are all single-use and must be bought pre-sterilised.
The surgical room should have good air cleanliness and hard non-porous surfaces. All surfaces should be wiped down with isopropyl alcohol at least twice and an ozone lamp may be used15 to sterilise the room overnight prior to surgery.
Prior to surgery all personnel should sterilise themselves using chlorhexidine body wash (commercially sold as Hibiscrub). Masks, haircaps and sterile gloves should be worn. All personnel apart from the patient should be wearing surgical gowns. The patient should be covered in drape around the parts of their body that are not involved in surgery (although this may not be practical in self-surgery).
Pre-operative care
Although some sources recommend intravenous antibiotics or antibiotic wound irrigation (probably simply because it is common practice), evidence does not support this16. Systemic antibiotics have a wide range of side effects and should be avoided unless there is reason to suspect an infection. During procedure and especially prior to suturing, the tissue should be irrigated and blood washed out with sterile saline or 0.05% chlorhexidine solution.
Anaesthesia can be achieved via the use of an amino amide anaesthetic such as Lidocaine or Bupivacaine. Although the risk is low, it must be kept in mind that these medications may cause toxicity if used in large quantities17. Lidocaine has a quick onset whereas bupivacaine requires 6-10 minutes to take effect but lasts much longer (about 6 hours)18.
For these reasons, an ideal anaesthetic for orchiectomy is a 1:2 ratio mixture of 2% lidocaine and 0.5% bupivacaine1920. A 25G needle should be aspirated (pull back on plunger and see that no blood comes out to make sure injection is not being made into a blood vessel) and used to administer ~10ml of anaesthetic to each spermatic cord, as well as some subcutaneously at the site of incision. Sensory blockade should be tested21, for example by lifting the skin with forceps. Some additional anaesthetic may be sprayed/squirted onto the tissue throughout the operation.
Operation
The scrotum should be shaved before procedure. A 2-4 cm vertical midline incision over the median raphe of the scrotum is made with a type 15 scalpel while a testicle is pushed towards the incision, with tension being applied to the skin. Next, the dartos muscle and tunica layers are dissected until the parietal layer of the tunica vaginalis is incised, which may be accompanied by a gush of fluid from the tunica vaginalis cavity. The testicle and cord are freed from the surrounding tunics and extracted via the incision. Dissection of the external spermatic fascia allows for lengthening of the spermatic cord. The testicle and spermatic cord should be removed with as much cord length as possible, as residual cord tissue can be bothersome postoperatively.
Separate the cord into two bundles. Starting with the vas deferens, double clamp proximally and single distally with Kelly Haemostatic clamps. The vas deferens and the vascular bundle are both ligated with a stick tie using 2-0 Vicryl, followed by a proximal free tie. The testicle may then be cut and, once haemostasis is ensured, the spermatic cord may be allowed to retract. The procedure is performed bilaterally.
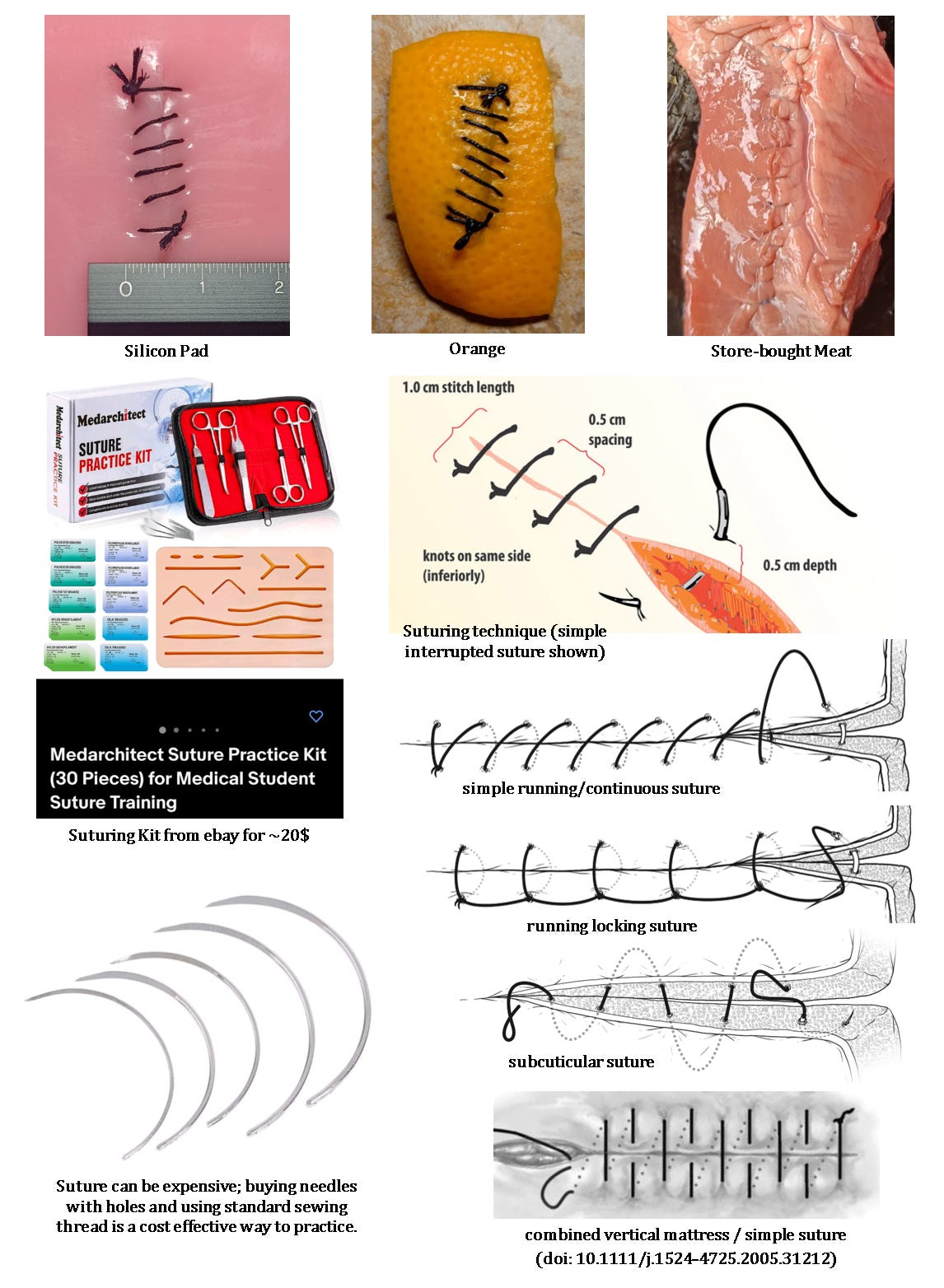
Haemostasis of the scrotal tissue can be achieved with cautery. The sack should be irrigated with saline and 0.05% chlorhexidine prior to closure. The dartos layer is sutured together with the septum (see above) using 4-0 Vicryl simple running suture. The sack is pressed down to remove any trapped air, then the skin is sutured with 4-0 Monocryl using a simple running suture. Care is taken not to remove any scrotal skin or dartos tissue, which may be used for vaginoplasty in the future. Triclosan-coated Vicryl (“Vicryl plus Triclosan”) may be used to reduce risk of infection. Finally, skin glue and a large tegaderm plaster may be applied.
Post-operative care
In order to avoid haematoma formation a scrotal support and compression should be used22. Tight underwear should be worn and ice used regularly for pain/inflammation management. NSAID’s such as ibuprofen are recommended, although in cases of more severe pain a narcotic analgesic such as oral codeine (which unlike the other two can often be purchased OTC), morphine or oxycodone may be used.
Topical antiseptics such as chlorhexidine23,cetrimide24, benzoyl peroxide25, zinc oxide, octenidine and povidone iodine26 all have limited skin penetration but can be effective for disinfection of surface layers (most can be found at a pharmacy). Chlorhexidine provides bactericidal activity for 24 hours after a 2-minute application, making it a useful antiseptic for anticipated long procedures27. A topical antibiotic cream such as Gentamicin and Clindamycin may also be effective.
In case of infection systemic oral antibiotics may be used. If no immediate improvement is seen, seek professional medical treatment immediately. In case of haematoma28, the majority of haematomas resolve without medical treatment. The recommended treatment for a venous hematoma is watchful waiting, anti-inflammatory medication (ibuprofen), and a compressive dressing. The haematoma will liquefy in 7-14 days after formation and will slowly dissolve and be absorbed by the body. The scrotal skin will go through colour changes as the hematoma is slowly dissolved. If the patient is very symptomatic from a venous haematoma then seek professional medical treatment immediately (a surgical drain may need to be performed).
Post-operative haematoma:
The following are to be expected after surgery:
Some discomfort.
Bruising and discoloration of your scrotum and the base of your penis for 1 to 2 weeks.
Some swelling of your scrotum.
Some thin, clear, pinkish fluid draining from the incision for a few days.
The following can be a sign of infection:
Increased pain, swelling, warmth, or redness.
Red streaks leading from the incision.
Pus draining from the incision.
A fever.
Antiandrogens should be discontinued. Surgical dressings can be removed on postoperative day two. At that stage, patients may shower, but should wait 1 month before taking baths or swimming. Heavy lifting should also be avoided for 1 month. Avoid all sexual activity including masturbation for at least a week. The majority of healing should have occurred within 3-4 weeks.
Principles of surgery
Stoker’s “Basic Surgical Skills and Techniques” is an excellent starting source29. William Halsted devised a set of basic surgical principles in the late 19th Century, known as Halstead’s Principles303132. They are:
Gentle tissue handling and anatomical dissection of tissue, including appropriate use of instruments. Tissue should not be grasped with serrated forceps and scalpel cuts should be direct and precise (not like using a paintbrush).
Minimise tissue tension through correct selection of suture materials, suture patterns and the skillful placement of sutures. The degree of tension in a suture is an important factor in the process of wound healing. If there is too much tension, blood flow is restricted which may result in necrosis. This will result in wound breakdown.
Preservations of blood supply, which is also achieved through careful dissection and the correct tightness of sutures. Better blood supply ensures faster healing.
Accurate tissue apposition by bringing the edges of tissues together neatly. This is achieved by the correct selection of suture materials and suture patterns and correct placement of sutures
Effective haemostasis through the skillful use of ligatures, suture material and clamps. Haemostasis is the process of preventing bleeding. Electrocautery is an extremely effective method, although chemical cautery is also an option.
Strict asepsis, which can be achieved via the use of PPE, sterilisation techniques and antiseptic agents. This was discussed earlier in the document.
Elimination of dead space by closure of the appropriate number of layers (both dartos and surface layer for orchiectomy), irrigation of the wound with saline and compression of scrotum prior to placement of final suture to let out any air.
Suturing
The best way to learn suturing is by watching videos, imitating, and then practicing over and over again. There are also some excellent paper/articles33343536.
“Suture Techniques Course Video” www.youtube.com/watch?v=Akyr4zlBS9E
“How to Tie Surgical Knots: Instrument tie” www.youtube.com/watch?v=cEis_EH2bQQ
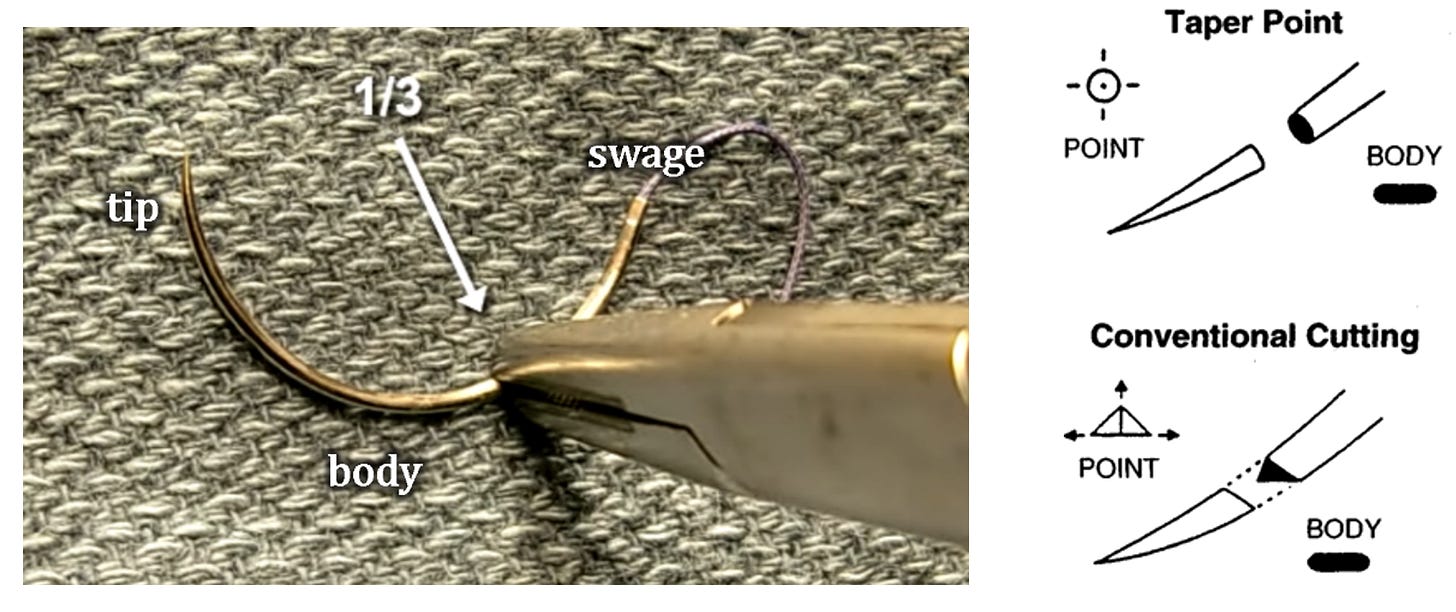
The needle should be held at the body, approximately 1/3rd away from the swaged end. A cutting needle should be used for suturing (as opposed to a tapered needle) because it is more durable and will help to thread suture through the skin cleanly. Needle should be inserted approximately 90deg to the skin.
For suture practice, a kit may be purchased cheaply online, which includes a silicon practice pad. Fruits such as oranges may also be used. However, fruits are easy to accidentally cut through and do not have material properties similar to real skin – for this reason, store-bought chicken leg (with skin) or other types of meats are highly recommended.
Care must be taken to not overtighten the suture and to correctly level the skin.
Ligation
Meticulous haemostasis (or lack thereof) is likely to be the primary factor causing post-surgical complications. Ligatures must be extensively practiced. A reminder that the vascular bundle and vas deferens of each cord will require a stick tie, with a second proximal free tie, making 8 ties in total. The ties can be made either with a two-handed, one-handed or instrument tie (same as for suturing) technique.
“Ligation Of Blood Vessel ( Regular Tie Technique)”
www.youtube.com/watch?v=7eSmOSQkAz8
“Ligation Of Blood Vessel ( Stick Tie Technique)”
www.youtube.com/watch?v=5-E57ttwyUI
Another important thing to keep in mind is the number of throws used when tying ligatures or suturing3738:
Cautery
If it can be afforded (>400$) a needle electrocautery machine should be used to assist with the surgery. However, this may be too expensive of a luxury for some. Single-use cautery pens can be bought for ~10$ and can be used to assist with minor bleeding. Perhaps a soldering iron with sterile tip could be used… probably a bad idea.
“How to Control Bleeding with a Battery Cautery Unit”
www.youtube.com/watch?v=elw_PhiDITw
Another form of cautery is chemical cautery, for example via the use of silver nitrate sticks. This however is usually reserved for non-surgical use and is strongly advised against39. Antihemorrhagic agents such as styptic pencils may reduce bleeding, but are also not recommended.
Orchiectomy videos:
“Simple orchiectomy for transgender patients” simple, midline incision
“Simple orchiectomy step-by-step technique” simple, bilateral incision
“Total Orchiectomy final” simple, midline incision
“Simple Bilateral Orchiectomy, type of orchiectomy for transgender” simple, midline incision
Additional resources:
WHO Global guidelines for the prevention of surgical site infection, 2nd ed.
Orchiectomy, r/TransSurgeriesWiki
https://www.reddit.com/r/TransSurgeriesWiki/wiki/srs/introduction/#wiki_orchiectomy
“Self-performing orchiectomy”, written by Effy
https://ksenia.sexy/en/self-orchiectomy
Cases of self-orchie:
huamoya123
twitter.com/huamoya123/status/1456833099166216198
Orchieanon
https://archived.moe/lgbt/thread/22577899/
https://archived.moe/lgbt/thread/22572346/
Effy
https://archived.moe/lgbt/thread/14909833
Orchiectomy. Wikipedia; 2022.
Inguinal Orchiectomy. Wikipedia; 2022.
Hehemann, M. C.; Walsh, T. J. Orchiectomy as Bridge or Alternative to Vaginoplasty. Urol. Clin. North Am. 2019, 46 (4), 505–510. https://doi.org/10.1016/j.ucl.2019.07.005.
The Male Genital Organs - Human Anatomy. https://theodora.com/anatomy/the_male_genital_organs.html (accessed 2022-10-07).
Liu, L. Chapter 1 - Applied Anatomy of the Scrotum and Its Contents. In Scrotoscopic Surgery; Yang, J., Ed.; Academic Press, 2019; pp 1–8. https://doi.org/10.1016/B978-0-12-815008-5.00001-7.
Team, H. J. Scrotum Anatomy, Scrotum Function and Causes of Lump or Pain in Scrotum. Health Jade, 2019.
Francis, C.; Grober, E.; Potter, E.; Blodgett, N.; Krakowsky, Y. A Simple Guide for Simple Orchiectomy in Transition-Related Surgeries. Sex. Med. Rev. 2020, 8 (3), 492–496. https://doi.org/10.1016/j.sxmr.2019.11.004.
Effy, T. Self-performing orchiectomy. https://ksenia.sexy/en/self-orchiectomy (accessed 2022-10-08).
Smith (Jr.), J. A.; Howards, S. S.; Preminger, G. M.; Dmochowski, R. R. Hinman’s Atlas of Urologic Surgery; Elsevier, 2017.
Glenn’s Urologic Surgery - Google Books. https://books.google.co.uk/books/about/Glenn_s_Urologic_Surgery.html?id=GahMzaKgMKAC&source=kp_book_description&redir_esc=y (accessed 2022-10-12).
World Health Organization. Decontamination and Reprocessing of Medical Devices for Health-Care Facilities; World Health Organization, 2016.
Disinfection and sterilization in health care facilities: what clinicians need to know - PubMed. https://pubmed.ncbi.nlm.nih.gov/15356786/ (accessed 2022-10-08).
Cook, R. K.; McDaniel, J.; Pelaez, M.; Beltran, T.; Webb, O. Use of a Pressure Cooker to Achieve Sterilization for an Expeditionary Environment. J. Spec. Oper. Med. Peer Rev. J. SOF Med. Prof. 2021, 21 (1), 37–39. https://doi.org/10.55460/WPGC-A599.
Using a Pressure Cooker as an Autoclave. EPI Newsl. 1984, 6 (6), 5–8.
Szeto, W.; Yam, W. C.; Huang, H.; Leung, D. Y. C. The Efficacy of Vacuum-Ultraviolet Light Disinfection of Some Common Environmental Pathogens. BMC Infect. Dis. 2020, 20, 127. https://doi.org/10.1186/s12879-020-4847-9.
Barnes, S.; Spencer, M.; Graham, D.; Johnson, H. B. Surgical Wound Irrigation: A Call for Evidence-Based Standardization of Practice. Am. J. Infect. Control 2014, 42 (5), 525–529. https://doi.org/10.1016/j.ajic.2014.01.012.
Mehra, P.; Caiazzo, A.; Maloney, P. Lidocaine Toxicity. Anesth. Prog. 1998, 45 (1), 38.
Helgeson, L. E.; Sinatra, R. S. Overview of Local Anesthetics. In The Essence of Analgesia and Analgesics; Watkins-Pitchford, J. M., Jahr, J. S., Sinatra, R. S., Eds.; Cambridge University Press: Cambridge, 2010; pp 267–273. https://doi.org/10.1017/CBO9780511841378.064.
Lee, K.; Chung, J. M.; Lee, S. D. The Safety of a Mixture of Bupivacaine and Lidocaine in Children after Urologic Inguinal and Scrotal Surgery. Investig. Clin. Urol. 2018, 59 (2), 141–147. https://doi.org/10.4111/icu.2018.59.2.141.
Shin, Y. S.; Doo, A. R.; Park, J. K. Let’s Take Advantage of Mixtures of Bupivacaine or Ropivacaine in Urologic Inguinal and Scrotal Surgery. World J. Mens Health 2018, 36 (2), 171–172. https://doi.org/10.5534/wjmh.180009.
Curatolo, M.; Petersen-Felix, S.; Arendt-Nielsen, L. Sensory Assessment of Regional Analgesia in Humans: A Review of Methods and Applications. Anesthesiology 2000, 93 (6), 1517–1530. https://doi.org/10.1097/00000542-200012000-00025.
Oesterling, J. E. Scrotal Surgery: A Reliable Method for the Prevention of Postoperative Hematoma and Edema. J. Urol. 1990, 143 (6), 1201–1202. https://doi.org/10.1016/s0022-5347(17)40224-2.
Herruzo-Cabrera, R.; Garcia-Torres, V.; Rey-Calero, J.; Vizcaino-Alcaide, M. J. Evaluation of the Penetration Strength, Bactericidal Efficacy and Spectrum of Action of Several Antimicrobial Creams against Isolated Microorganisms in a Burn Centre. Burns J. Int. Soc. Burn Inj. 1992, 18 (1), 39–44. https://doi.org/10.1016/0305-4179(92)90118-e.
Hussain, S. N.; Rabbain, M.; Amir, M. F. Study of Percutaneous Absorption of Diclofenac Diethylamine in the Presence of Cetrimide through Hairless Rabbit Skin. J. Res. Sci. 2006, 17 (1), 45–52.
Seubert, S.; Seubert, A.; Ippen, H. [Penetration of benzoyl peroxide in the skin]. Hautarzt Z. Dermatol. Venerol. Verwandte Geb. 1984, 35 (9), 455–458.
Herruzo-Cabrera, R.; Garcia-Torres, V.; Rey-Calero, J.; Vizcaino-Alcaide, M. J. Evaluation of the Penetration Strength, Bactericidal Efficacy and Spectrum of Action of Several Antimicrobial Creams against Isolated Microorganisms in a Burn Centre. Burns J. Int. Soc. Burn Inj. 1992, 18 (1), 39–44. https://doi.org/10.1016/0305-4179(92)90118-e.
Bednarek, R. S.; Nassereddin, A.; Ramsey, M. L. Skin Antiseptics. In StatPearls; StatPearls Publishing: Treasure Island (FL), 2022.
Risk of Bleeding After Vasectomy. His Choice. https://www.bestvasectomy.com/risk-of-bleeding-after-vasectomy/ (accessed 2022-10-10).
Jain, S. K.; Stoker, D. L.; Tanwar, R. Basic Surgical Skills and Techniques; JP Medical Ltd, 2018.
Halsted’s principles - Wikipedia. https://en.wikipedia.org/wiki/Halsted's_principles (accessed 2022-10-10).
Memorize 7 Principles To Be Smooth Operator. https://www.veterinarypracticenews.com/memorize-7-principles-to-be-smooth-operator/ (accessed 2022-10-10).
Surgical principles // WVS Academy. https://wvs.academy/learn/companion-animals/spay-neuter/preparation-and-principles/surgical-principles/surgical-principles (accessed 2022-10-10).
Suturing techniques | DermNet. https://dermnetnz.org/topics/suturing-techniques (accessed 2022-10-10).
Veeraraghavan, R. Wound Closure and Care in Oral and Maxillofacial Surgery. In Oral and Maxillofacial Surgery for the Clinician; Bonanthaya, K., Panneerselvam, E., Manuel, S., Kumar, V. V., Rai, A., Eds.; Springer Nature: Singapore, 2021; pp 217–237. https://doi.org/10.1007/978-981-15-1346-6_11.
Moy, R. L.; Waldman, B.; Hein, D. W. A Review of Sutures and Suturing Techniques. J. Dermatol. Surg. Oncol. 1992, 18 (9), 785–795. https://doi.org/10.1111/j.1524-4725.1992.tb03036.x.
Sutures and knots | Bristol Veterinary School | University of Bristol. https://www.bristol.ac.uk/vet-school/research/comparative-clinical/veterinary-education/clinical-skills-booklets/sutures/ (accessed 2022-10-10).
Silver, E.; Wu, R.; Grady, J.; Song, L. Knot Security- How Is It Affected by Suture Technique, Material, Size, and Number of Throws? J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2016, 74 (7), 1304–1312. https://doi.org/10.1016/j.joms.2016.02.004.
Tidwell, J. E.; Kish, V. L.; Samora, J. B.; Prud’homme, J. Knot Security: How Many Throws Does It Really Take? Orthopedics 2012, 35 (4), e532-537. https://doi.org/10.3928/01477447-20120327-16.
Silver Nitrate and Wound Care: The Use of Chemical Cauterization. WoundSource. http://www.woundsource.com/blog/silver-nitrate-and-wound-care-use-chemical-cauterization (accessed 2022-10-10).










Dear Author,
As a medical professional, I find myself both horrified and deeply impressed by your story. Rather than offering the expected lecture on medical risks—which I’m sure you are already well aware of, given the life-threatening nature of these risks and the dangers of unattended gender dysphoria —I’ll focus on a single point.
What you accomplished is extraordinary. Your level of preparation, medical knowledge, and months of hands-on practice are unparalleled, even among young doctors. Moreover, your methods of material collection, citation style, and writing skills are of a caliber typically seen in academic publishing.
Therefore, I must emphasize that your story is far from an easy or safe one to replicate.
With all my respect and kindness, Kat
Informative site, I congratulate you!